‘Humanised’ Mice Developed To Improve Immunotherapy Testing
Animal testing in determining a product’s efficacy on humans has always been subjected to debate. However, it sure proved itself helpful in the development of immunotherapy cures.
Testing cancer cures has been dependent on mouse models by growing tumours on mice and figuring out how to eradicate them. Tumours are transplanted into the mice, bringing down the rodent’s immune system so as not to affect the tumour’s growth.
A new development has been made to improve the responses and results of mice testing with XactMice which are basically lab mice grown with “humanised” mouse immune systems. Developed by the University of Colorado Cancer Center, XactMice is infused with human blood stem cells to grow a humanised immune system before the tumour is transplanted to the mouse.
Immunotherapy is known to strengthen the human immune system to attack cancer from within. This new mouse model means that testing for cures will be more accurate, since researchers will now be dealing with a human-like immune system with a human tumour. Antonio Jimeno, a senior author of University of Colorado School of Medicine Head and Neck Cancer Clinical Research Program, said that this is a huge leap forward in immunotherapy research.
“One of the reasons that anti-cancer immune therapies have been difficult to develop is that perhaps we haven’t had adequate models. Now we have a model that will enable some of those studies,” said Jimeno in a post by Science Codex. Jimeno’s team was the one that performed the work, collaborating with the Gates Center for Regenerative Medicine.
Dr Yosef Rafaeli, a corresponding author of the study and a faculty member in the Dermatology Department of Gates Center, said that the team did a bone marrow transplant on the mice. The mice were treated with radiation to take down its existing blood and cell system. Human stem cells from human cord blood were then introduced to replenish the blood system. “After a few months, the mice became chimeras – with human blood cells and hence a human immune system,” said Rafaeli.
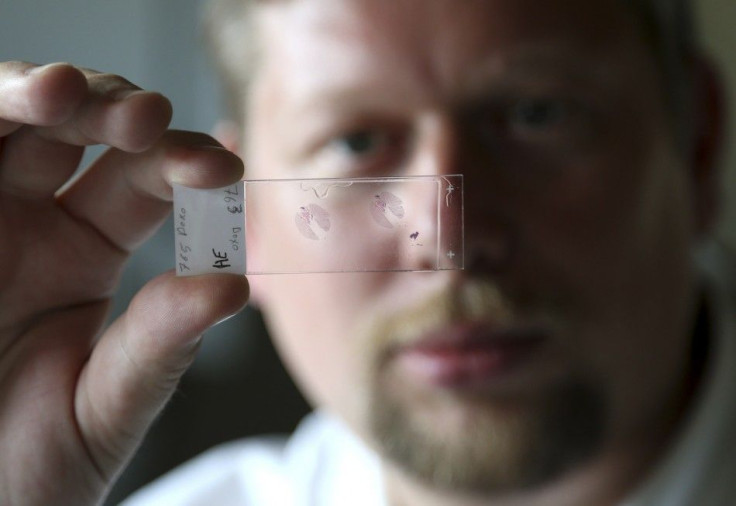
According to a post by Science 20, there is a protocol for testing these said humanised mice for applications in human patients. First, the researchers recruit patients at the CU Cancer Center, then small tumour samples are taken from melanoma, particularly from head and neck cancer patients.
Next, blood stem cells from these cancer patients will be used to “humanise” the mice, then the tumours from the patients will be transplanted and grown on the mice that matches the patients’ immune systems. Once the tumours are developed, the mice will be treated with immunotherapy, with the results to be compared with the human patients’.
“This might be a better model for several areas of cancer (and non-cancer) research, and since each mouse provides a lot of information, we will be able to do more with less mice,” said Jimeno.
Immunotherapy is a current popular cancer cure because of the positive results it brings. Biotech companies around the world are developing their own immunotherapy cures to attack different kinds of tumours around the body. California-based Nascent Biotech, Inc. (OTC: NBIO) is responsible for the brain-cancer cure Pritumumab, a natural human antibody that has been used to treat 250 cancer patients.
Pritumumab was derived using proprietary technology from a B-cell isolated from a tumor draining lymph node of a patient with cervical cancer. It targets ectodomain vimentin that is found on the cell surface of many kinds of adenocarcinomas that include brain cancers and melanoma. So far, Phase II of clinical trials of Pritumumab in Japan gave an overall response rate of 25 to 30 percent, with survivors going way past 5-years post-treatment. If able, Nascent Biotech could use XactMice to further advance their researches on brain cancer cures.
To contact the writer, email: v.hernandez@ibtimes.com.au





















