New microscope being developed allows detection of cancer without biopsy
To help medical practitioners distinguish between cancerous cells and healthy cells both inside the operating room or an office setting, mechanical engineers from the University of Washington are developing a handheld microscope. The device would allow surgeons to see at the cellular level during surgery to help them determine when to stop cutting cancerous cells.
When removing tumour, surgeons would definitely not want to leave cancerous material behind to protect healthy cells and minimize harm. In the case of a brain surgery, once doctors have opened up the patient’s skull, they do not have enough time to send brain tissues to a pathology lab to distinguish between healthy and cancerous brain cells. When taken to the lab, tissues are usually frozen, cut, stained, placed on slides and investigated using large microscopes. The handheld microscope is being developed by the university, in collaboration with Memorial Sloan Kettering Cancer Center, Stanford University and the Barrow Neurological Institute.
The handheld device would enable surgeons to go beyond on-the-spot analysis made during the procedure. Jonathan Liu, assistant professor of mechanical engineering at the university and senior author of the study, explains that “Surgeons don’t have a very good way of knowing when they’re done cutting out a tumor … They’re using their sense of sight, their sense of touch, pre-operative images of the brain – and oftentimes it’s pretty subjective.”
He adds that giving surgeons the ability to zoom and see at the cellular level while performing surgery would really be a big help for them to differentiate accurately between tumour and normal tissues. This, in turn, would improve patient outcomes.
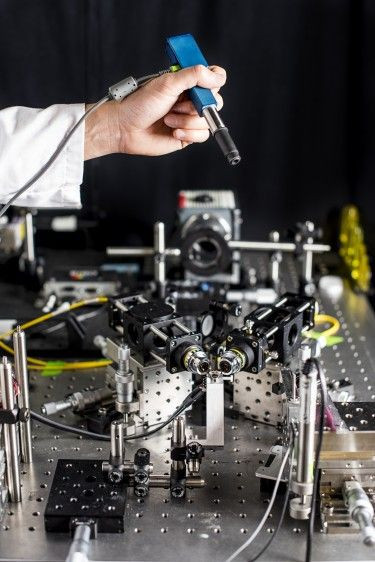
Liu says that the small microscope is just as big as a pen. He adds that researchers hope to start testing the new technology, as a cancer-screening tool, in clinical settings in 2017, reports Phys.org. The university explains how the device works in a paper published in the January issue of the Biomedical Optics Express journal.
Milind Rajadhyaksh, co-author, points out that in the last couple of decades, microscope technologies developed are costly and quite large, about the size of a small dental x-ray machine or a hair dryer. Although he acknowledges the need to create smaller microscopes, the associate faculty member of dermatology service at the Memorial Sloan Kettering Cancer in New York City, admits shrinking the vital lab equipment often sacrifices some aspects such as image quality or performance.
He continues, “We feel like this device does one of the best jobs ever – compared to existing commercial devices and previous research devices – of balancing all those tradeoffs.”
The microscope they are developing uses a dual-axis confocal microscopy to light up and provide a clearer image through opaque tissue. It is also capable of capturing details up to half millimetre beneath the tissue surface, a place where some types of cancerous cells begin.





















