In Nigeria, African Researchers Blaze A Trail In Virus Fight
"Strong people don't put others down -- they lift them up."
So says the discreet sign at the entrance to one of the most remarkable research facilities in Africa.
Run by a Cameroon-raised, Harvard-trained molecular biologist, the African Centre of Excellence for Genomics of Infectious Diseases (ACEGID) has been at the forefront in the fight of killer diseases such as Ebola, Lassa fever -- and now COVID-19.
The force behind the lab is Professor Christian Happi, who has a steely belief in catapulting young African scientists to the top of scientific research.
"As long as Africa fails to make intellectual contributions, it will always be told what to do," he said.
ACEGID'S 52-year-old director has already set down a marker in the battle against coronavirus by devising a low-cost test for the highly contagious disease.
"I want to develop simple, inexpensive solutions that are aligned to Africa and our environment," he said, speaking in his office, its walls decorated with diplomas, awards and photos of his family.
Happi founded his laboratory in 2016 in an ageing building at Redeemer's University in Ede, an unassuming town in southwest Nigeria, with the help of funding from the World Bank and Nigerian and foreign philanthropists.
Since then, nearly 1,000 scientists, most of them Nigerians and the others from West Africa, have passed through its doors to gain top-level experience in biochemistry and genomics.
A gleaming new building -- "the biggest genomic research centre in Africa" -- is scheduled to open by the end of the year in the tropical forests around Ede.

"It makes sense to be here in Nigeria. This country is the giant of Africa -- if it fails, the entire continent will fail with it," said Happi.
Nigeria is not only home to around 200 million people -- its vast territory, stretching from the edge of the Sahara to the tropical coastline of the Gulf of Guinea, also hosts epidemics ranging from malaria and typhoid to meningitis, cholera and yellow fever.
This year, every mind at ACEGID is focussed on COVID-19.
Nigeria has officially recorded around 800 deaths and more than 30,000 cases, but the true extent of infection is likely to be much wider, given huge, dense populations in Lagos, Ibadan, Abuja and Kano, where social distancing is almost impossible.
The country carries out on average only 3,000 tests per day -- a drop in the ocean for what is needed.
Happi's team in Ede has developed a fast-track test that has already been certified by the US Food and Drug Administration (FDA) and is currently being vetted for use in Nigeria and across Africa.
The test -- which resembles the kind of simple dip stick used for pregnancies -- costs around $3 (2.60 euros) each, against around $100 for polymerase chain reaction (PCR) tests, a method that requires an expensive, well-equipped lab.
"I'm not interested in the big PCR machines used in Europe or the United States, which no public hospital here can afford," said Happi, striding between laboratories.
"I want tests that a grandmother in a village can get done in her rural clinic."
Happi's quest for simplicity is being conducted with state-of-the-art equipment.
It was the first lab to sequence the genetic profile of the new coronavirus in Africa -- a feat that took just a few days after the first case of the disease showed up in Lagos in early March.
The speed was "incredible", said Chikwe Ihekweazu, head of the Nigeria Centre for Disease Control (NCDC).
"Previously we would have done it in Europe or in the States."
There are many advantages to having research excellence on one's doorstep.
"The virus can evolve rapidly and in many ways. With genomic sequencing you have the ability to study that in real time," said Ihekweazu.
"People might have thought that this work was impossible in Africa," Happi said last month in the prestigious science journal Nature.
"But we are demonstrating that the continent's scientists can generate crucial data in the global fight against COVID-19 -- as well as contributing to the field of genomics."
Happi and Ihekweazu, who are of the same age, know each other well and have a common foe.
"Professor Happi is a tough character -- we have a lot of debates, but both of us know that we are committed to Africa and to the country," said Ihekweazu.

In Cameroon, where he caught malaria as a child, Happi trained in biochemistry before going to Britain in 1998 at the age of 30 to attend a conference on malaria.
At the time, Africa was almost literally the country cousin in terms of its status in world research, and Happi recalled arriving at London's Heathrow Airport -- "a little African with a big suitcase, and feeling a little lost".
But he made a big impact in the conference at Oxford, where as one of the few African attendees he put forward "a bunch of wacky ideas" for using gene technology in vaccines.
Such methods are at the heart of several COVID vaccines being researched today, but at the time such thinking was out of the mainstream, and Happi was snapped up by Harvard to carry out research there.
He studied and then taught there for a dozen years, specialising in malaria, a disease that claims nearly 400,000 lives each year, almost 100,000 of them in Nigeria alone.
"As long as research is not carried out on the continent, there will be no vaccine," said Happi. "You have to be here."
It wasn't his interest in malaria that brought him home, but Lassa fever -- a deadly haemorrhagic cousin of Ebola.
In 2007, learning about the disease that killed around 700 Nigerians each year, Happi was stupefied to find that tests for Lassa were sent to Germany. In the time it took to get the results back, 90 percent of patients had already died.
"It is completely unacceptable that a disease discovered in 1969 still does not have diagnostics in 2007," he said at the time.
He spent the next year raising funds and headed to Irrua, in southern Nigeria, where he built a lab.
There he trained two young people who were fresh out of high school in the basics of microbiology, and conducted Africa's first-ever home-grown tests for Lassa fever.
"There was nothing, no manpower or equipment," he recalled.
"There wasn't even electricity. We had to use a car battery to power the PCR machine!"
Today, Lassa tests are carried out much faster and with less trepidation. The disease, which is endemic to Nigeria, claims between 100 and 200 lives each year.
Bolstered by this experience, Happi founded ACEGID, which became a crucible of learning about African microbes -- he recently discovered the Ekpoma 1 and Ekpoma 2 viruses, among hundreds of viral strains that inhabit tropical forests in West Africa.
Despite these successes, the obstacles to setting down a solid foundation for African research are many.
Many scientists, doctors and health workers are lured abroad by the offer of higher pay and better working conditions.
"Young African students may be educated in the best universities of the world, but if there is no structure to welcome them in Africa once they have graduated, it's no good," Happi said.
Idowu Olawoye, 27, studied molecular biology and computer science in England before returning home in 2016.
He insisted that it was no problem for him to work in Ede, a small town that lies more than six hours by road from Lagos, Nigeria's vibrant economic hub.
"I really want to make an impact in my country," he said.
His role is to sift through genetic changes in a coronavirus sample that, when compared with other samples, show how the pathogen has spread.
"Look, here you can see on this graph... It's like you are reading its passport," he said.
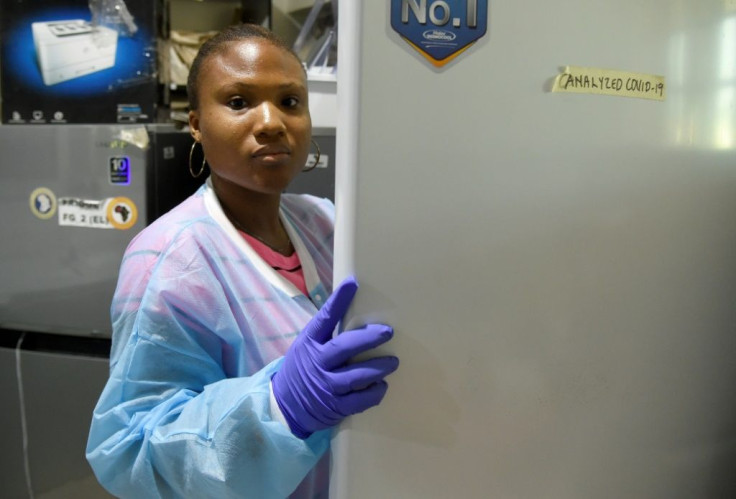
His colleague, Jessica Uwamibe, 29, a doctorate in molecular biology, has been working on the final touches to the COVID-19 test, and is now researching a vaccine based on the genetic profile of the virus found among Nigerian patients.
"Here we have the diseases -- and now we have the knowledge and the facilities," Uwamibe said. "Where else would I go?"





















